Realize Band Surgery
Here you’ll find information on:
- How it works
- Who is a good candidate?
- Pre-surgery considerations
- What to expect afterward
- Fills and adjustments
- Weight loss
- Eating afterward
- Risks
- Cost
The Realize Adjustable Gastric Band is a relatively new player in the world of gastric banding. Realize Band is the brand name of an adjustable gastric band developed in Sweden in 1985. Originally it was called the Swedish band. By 2006, 90,000 Swedish bands were sold outside the United States. The company changed the name to the Realize Band in 2007 around the same time that the device received approval from the U.S. Food and Drug Administration.
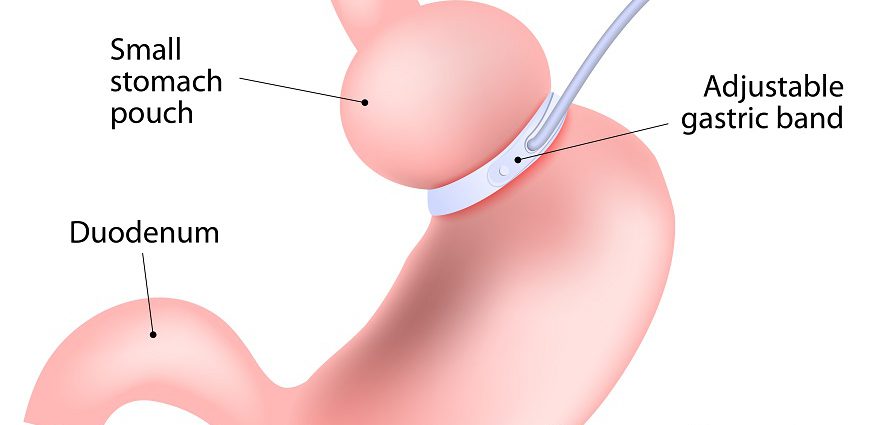
Similar to the Lap-Band system, the Realize Band is a restrictive type of weight loss surgery. It comprises two devices that are implanted at the same time during surgery.
How the Surgery Is Done
The band is made of a strong, flexible silicone. A bariatric surgeon would wrap the band completely around the upper part of your stomach. This creates a small pouch and a narrow passage to the lower stomach. This small passage delays the emptying of food from the pouch and causes a feeling of fullness.
A soft balloon inside the band comes into direct contact with the stomach. This balloon holds up to 1.8 teaspoons of saline solution.
The second implant is called the Realize Injection Port, and it is attached to the abdominal wall under the skin. It is used for fills or adjustments. During fills, your surgeon injects saline into the port to tighten or loosen the band. These adjustments are made periodically based on weight loss, food cravings and other physical reactions to the surgery. The Realize Band and port are connected by a hollow tube.
Adjustable gastric banding with the Realize Band is usually performed laparoscopically, meaning that your surgeon makes small incisions as opposed to one large incision. He or she inserts a viewing tube with a small camera (laparoscope) and other tiny instruments into these small incisions to perform gastric banding.
Gastric banding surgery with the Realize Band takes about one to one-and-a-half hours to perform. It can be done on an outpatient basis or may require a one-day hospital stay.
Who Is a Good Candidate?
The National Institutes of Health (NIH) requirements for adjustable gastric banding with the Realize Band are the same as for other weight loss surgeries. They include:
- A body mass index (BMI) greater than 40. This is the equivalent of being about 100 pounds overweight for men and 80 pounds overweight for women. There is no upper weight limit for people considering gastric banding. A BMI takes height and weight into account to measure body fatness, and a BMI of 30 or above in adults is considered obese. [Read more about body mass index, and measure your own with our BMI calculator.]
- A BMI of at least 35 in the presence of other obesity-related illnesses, such as diabetes, high blood pressure and high cholesterol.
- A history of obesity with failing conservative weight loss methods, including supervised diet, exercise and behavior modification programs.
- Being the right age. The NIH states that a person must be 18 to undergo gastric banding, but adolescents under 18 may be candidates for weight loss surgery if they meet certain criteria.
Adjustable gastric banding with the Realize Band may also be an option for people for whom the more invasive gastric bypass surgery is too risky.
Some people may not be good candidates for adjustable gastric banding with the Realize Band, including those with the following conditions or issues.
- Inflammation of the digestive tract (such as from ulcers, severe inflammation of the lining of the esophagus, the tube that carries food from the throat to the stomach or Crohn’s disease).
- Severe heart or lung disease
- Upper digestive tract bleeding
- Portal hypertension, an increase in the pressure within the vein that carries blood from the digestive organs to the liver (the portal vein). Caused by a blockage in the blood flow through the liver, the increased pressure causes large veins to develop across the esophagus and stomach to bypass the blockage. Portal hypertension is usually caused by cirrhosis of the liver (when scar tissue replaces the normal liver tissue).
- Abnormal digestive tract anatomy
- Cirrhosis
- Chronic pancreatis or inflammation of the pancreas (a large gland behind the stomach and close to the duodenum).
- Infection
- Allergies to implant materials
- Use of steroids for a long period of time or within 15 day of the surgery
- Current pregnancy
- Unwillingness or inability to make necessary changes to eating and behavior
Check with your surgeon to see if any of these restrictions apply to your situation, as some exceptions may apply.
Pre-Surgery Considerations
Regardless of the surgical method chosen, preparing for weight loss surgery starts with a lifelong commitment to the dietary and lifestyle changes you require for success. Weight loss surgery is not a quick fix, nor is it a decision to enter into lightly. Once you have made the decision together with your surgeon and your family members, the preoperative evaluations can begin. These may include:
- Meeting with a registered dietician to discuss how your diet needs to change both before and after weight loss surgery.
- A comprehensive psychological evaluation
- An upper endoscopy exam or a barium swallow, to make sure no polyps, tumors, ulcers or bacteria that cause ulcers are in your stomach.
- Additional pre-operative evaluations may be necessary for the heart and lungs.
- Telling your surgeon about any medications you are taking or plan to take throughout recovery. Vitamins, minerals and herbs also interact with medications. Don’t leave anything out.
Some of the lifestyle changes can and should start before surgery, including:
- Quitting smoking for at least 30 days before and after weight loss surgery. Smoking increases the risk of complications, such as potentially fatal blood clots. Smoking also increases the risk of pneumonia and other lung problems after surgery. It can also affect wound healing of the incisions and increase the risk of infection.
- Not drinking alcohol for at least 48 hours before weight loss surgery.
- Losing 5 to 10 percent of excess body weight. People who lose a moderate amount of weight before bariatric surgery have a shorter hospital stay and more rapid postoperative weight loss, according to a study in Archives of Surgery.
- Getting a head start on the new way of eating. In the weeks leading up to your surgery, start eating several small, balanced meals each day, don’t snack between meals, aim for sipping eight cups (64 ounces) of low-calorie, non-carbonated fluids each day, take small bites and chew each bite slowly and carefully.
- Consider starting a high-protein liquid diet in advance of Realize Band surgery, as this diet will let your surgeon better visualize the stomach during surgery.
- Talking with your health care team about what, if any, vitamin and mineral supplements to take prior to surgery.
- Learning about the risks and requirements of the Realize Band.
- Surrounding yourself with a network of supportive friends and family members who are rooting for your success. This can also include participating in live or online support groups.
What to Expect After Surgery
As with other weight loss surgeries, you must get re-used to eating solid foods after undergoing Realize Band surgery. This typically starts with a liquid-only diet for the first two weeks, to give swelling in the stomach a chance to go down. Experts recommend sipping at least eight cups of low-calorie, non-carbonated liquids during the first week or two after surgery to stave off dehydration. The liquid-only diet is followed by two or more weeks of semi-solid pureed foods, and then solids. Each surgeon likely has his or her own specific recovery diet.
Other considerations in the first week or two after surgery with the Realize Band may include:
- Not worrying about shoulder pain if it occurs a few days after surgery. After stomach surgery, many people report shoulder and neck pain that usually abates within a few days.
- Moving around, to reduce risk of pneumonia and blood clots after surgery.
- Exercising caution while bending at the waist or picking up heavy objects. An injury to the abdomen caused by improper bending or lifting may prolong recovery.
Fills and Adjustments
The stomach needs to heal from surgery before the first fill, so the first adjustment occurs around six weeks after surgery.
Many people who have undergone gastric banding surgery report that they can still eat relatively normal amounts of food until the first fill. The fills are done to make sure the band is not too tight or too loose and/or to encourage continued weight loss. The tighter the band, the more quickly the upper stomach fills up, and the less food you can eat. Band adjustments are painless, and your surgeon can make them during a regular office visit.
Studies of the Realize Band found that individuals required an average of four adjustments during the first year, two fills during the second year and two fills during the third year following surgery.
Weight Loss After Realize Band Surgery
The weight loss that occurs with adjustable gastric banding is more gradual than with some other weight loss surgeries. People who undergo gastric banding with the Realize Band report losing about one to two pounds per week.
A three-year study of the Realize Band showed that individuals lost about 40 percent of their excess weight by one year and 43 percent by three years after surgery. The average BMI dropped from 44 to 36 during the first year after surgery in this same study. On average, study participants maintained their reduced BMI three years after surgery.
Plastic surgery after massive weight loss may be necessary to remove excess skin and fat and create a more shapely body profile. Panniculectomy , thigh lift and body lift surgery are common post-bariatric procedures.
What You Should Eat After Surgery
After surgery you must be mindful about what you eat, how you eat and when you eat. This includes:
- Eating small meals each day. These meals should comprise about four ounces of food (half a cup).
- Not snacking between meals.
- Sipping eight, 8-ounce cups of low-calorie, non-carbonated beverages a day.
- Avoiding carbonated beverages, as carbonation may temporarily block the stoma (stomach outlet), causing discomfort and increased burping.
- Not drinking and eating at the same time, which may increase the chance of discomfort, regurgitation and vomiting.
- Changing your vitamins to chewable or liquid and crushing or breaking up medications so they are easier to digest.
- Chewing slowly and thoroughly and waiting a few minutes between each bite.
- Avoiding foods that may block the stoma. Some common culprits include bread, pineapple, celery, high-fiber foods and non-tender cuts of red meats.
- Heeding the warning signs. Pressure at the top of your stomach or hiccups means the upper stomach is full. Continuing to eat past these signals is not wise and may increase discomfort. Regurgitation, nausea, acid reflux, constipation and diarrhea may be signs to eat less, eat more slowly, chew thoroughly or eat different types of food. (Abdominal pain that lasts more than three hours is not normal. Contact your doctor if this occurs.)
Individual experiences with food and eating after Realize Band may vary. It is important to pay attention to your body and how you feel when you eat different foods at different times. Talk to your surgeon or a registered dietician about any problems you experience, as he or she will be able to offer tips on how to tweak your diet and eating habits. Keeping a journal of what you eat and how it makes you feel can aid in this effort.
Exercise is also an important part of life after Realize Band surgery. Aim for 20 to 30 minutes of aerobic activity three to four times a week. Think walking, cycling, swimming and jogging. Weight or strength training is also important. Clear it with your health care team before you begin weight training after surgery.
Realize Band surgery includes an interactive, Web-based support program. The program has four sections, covering nutrition, fitness, progress (such as weight loss and fill schedule) and obstacles. You can develop personalized eating and fitness plans with this program.
Realize Band Risks
Risks and complications include the following, and some may require a second operation.
- Bleeding
- Stomach pain
- Shoulder pain
- Pneumonia
- Complications due to anesthesia and medications
- Deep vein thrombosis
- Slippage of the band with persistent vomiting if behavioral changes are not made
- Erosion of the band into the inside of the stomach
- Spontaneous deflation of the band due to leakage
- Enlargement of the stomach pouch
- Blockage of the stoma (stomach outlet)
- Gastroesophageal reflux disease (GERD), when stomach contents rise up into the esophagus (tube that carries food from the mouth to the stomach)
- Infection
- Pulmonary embolism
- Stroke or heart attack
- Death
Cost of Realize Band Surgery
Realize Band surgery cost ranges from $16,000 to $25,000, depending on hospital fees and surgeon fees.The hospital will purchase the device, and it is usually billed to you as a part of the entire cost of the procedure.
Some insurance carriers may cover all or part of the surgery, so your first step is to check your health insurance plan.
(Read more about the cost of Realize Band surgery.)
Sources:
American Society for Bariatric Surgery. Brief History and Summary of Bariatric Surgery.Chapter 6. Gastric Banding
Still CD, Benotti P, Wood C, et al., Outcomes of preoperative weight loss in high risk patients undergoing gastric bypass surgery. Arch Surg. 2007;142:994-998
National Institute of Diabetes and Digestive and Kidney Disease website. Weight-control information network. Bariatric Surgery for Severe Obesity.
Realize Patient Guide, offered by Ethicon-Endo Surgery, manufacturer of the Realize Band